Are you dealing with unexpectedly heavy periods or vague pelvic pain that disrupts your daily routine? The uncertainty surrounding changes in your menstrual cycle can be overwhelming, leading to anxiety about your long-term health. In this detailed guide, we will explore the root causes of thick lining of uterus symptoms, helping you understand your body and discover effective, non-surgical ways to manage your condition.

What Does It Mean When the Lining of the Uterus Is Thick?
When we talk about the thick lining of uterus symptoms, we are primarily discussing a condition medically known as Endometrial Hyperplasia. The endometrium is the tissue lining the inside of your womb. Throughout your menstrual cycle, hormones like estrogen signal this lining to grow and thicken to prepare for a possible pregnancy. If conception doesn’t occur, progesterone levels rise, the lining sheds, and you get your period.
However, when this hormonal balance is disrupted—specifically when there is excess estrogen without enough progesterone to potentialize the shedding—the cells in the lining grow abnormally. This leads to a thickened endometrium. While often benign, understanding this condition is vital because, in some cases, it can be a precursor to uterine cancer.
This thickening isn’t just a number on an ultrasound report; it manifests physically. It often results in heavy menstrual bleeding, prolonged periods, and spotting between cycles. Identifying these signs early allows you to seek appropriate medical care. For many women, realizing that a thick uterus lining is the culprit behind their fatigue and pain is the first step toward better uterine health.
The Hormonal Connection: Estrogen and Progesterone
To understand why this occurs, we must look at the hormonal dance within your body. Estrogen is the hormone responsible for building the uterine lining. Progesterone is the hormone that stabilizes it and prepares it to shed.
In conditions like perimenopause, Polycystic Ovary Syndrome (PCOS), or obesity, your body might produce excessive amounts of estrogen. Without the balancing act of progesterone, the endometrium keeps building up, layer upon layer. This abnormal growth leads to the condition we are discussing. It is essential to learn that this hormonal imbalance is a common driver for both benign polyps and more complex hyperplasia.
Thick Uterine Lining Causes
The causes of a thickened lining are varied, but they almost always trace back to hormonal fluctuations. Identifying the root cause is the first step in determining the right treatment path.
1. Hormonal Imbalance (Estrogen Dominance)
This is the most frequent cause. As mentioned, when estrogen levels are high and progesterone is low, the lining overgrows. This is frequently seen in women approaching menopause (perimenopause) when cycles become irregular.
2. Polycystic Ovary Syndrome (PCOS)
Women with PCOS often have irregular periods or skip them entirely. Because the lining isn’t shed regularly, it accumulates and becomes abnormally thick.
3. Obesity
Fat tissue converts other hormones into estrogen. Therefore, carrying excess weight can lead to higher circulating estrogen levels, increasing the risk of endometrial hyperplasia.
4. Tamoxifen Use
This medication, often used to treat breast cancer, acts like estrogen in the uterus and can cause the lining to grow.
5. Uterine Fibroids and Adenomyosis
While Fibroids are muscular growths, they often coexist with a thick lining. Adenomyosis, a condition where the lining grows into the muscle wall of the uterus, also presents with a broadly enlarged and thickened appearance on scans. This is a key area of expertise for Dr. Samir Abdel Ghaffar, who treats these conditions without major surgery.
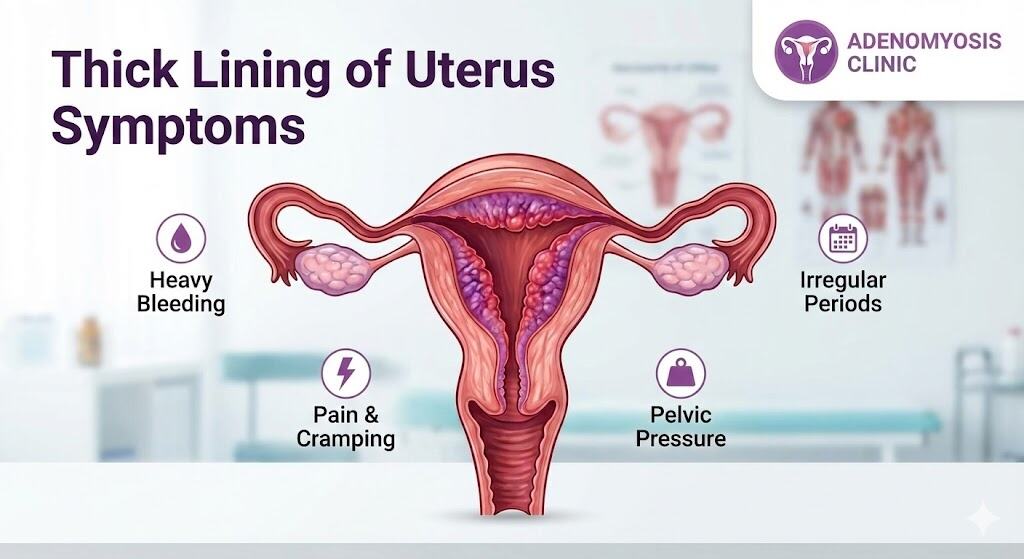
Thick Lining of Uterus Symptoms: What to Watch For
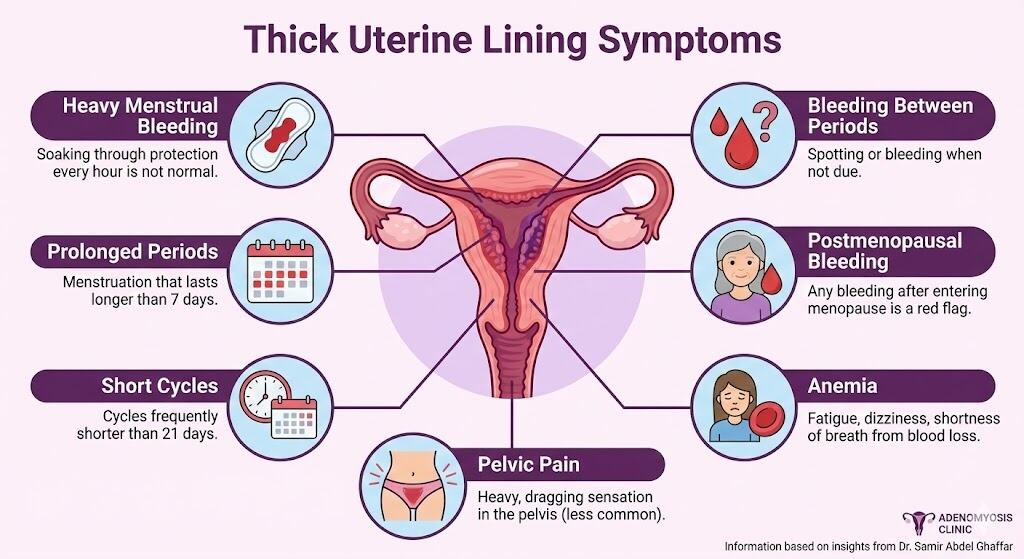
Recognizing the symptoms is crucial for early diagnosis. The signs of a thick lining are often mistaken for “just a bad period,” but they are your body’s way of signaling distress.
- Heavy Menstrual Bleeding: This is the hallmark symptom. Soaking through pads or tampons every hour is not normal.
- Prolonged Periods: Menstruation that lasts longer than 7 days.
- Cycles Shorter than 21 Days: Frequent periods mean the lining is unstable.
- Bleeding Between Periods: Spotting or bleeding when you are not due.
- Postmenopausal Bleeding: Any vaginal bleeding after you have entered menopause is a red flag and requires immediate investigation.
- Anemia: Due to chronic blood loss, you may feel fatigued, dizzy, or short of breath.
- Pelvic Pain: While less common than bleeding, a thick uterus lining or associated conditions like adenomyosis can cause a heavy, dragging sensation in the pelvis.
If you are experiencing these uncomfortable symptoms, it is time to consult an expert.
Does Thick Uterine Lining Mean Cancer?
This is the most frightening question for patients. The short answer is: Not necessarily.
Most cases of thickened endometrium are benign (non-cancerous). However, Endometrial hyperplasia is classified into different types based on the presence of atypical cells (cells that look abnormal under a microscope).
- Hyperplasia without Atypia: This is a simple overgrowth of normal cells. The risk of this turning into cancer is very low (less than 5%).
- Atypical Hyperplasia: This is more complex. The cells are abnormal and have a higher chance (around 30%) of developing into uterine cancer if left untreated.
Therefore, while a thick lining can be a symptom of cancer, it is more often a sign of a hormonal imbalance or benign hyperplasia. A biopsy is typically required to rule out cancerous changes definitively.
15 mm Endometrial Thickness Means…
Ultrasound measurements are the standard for assessing thickness. However, the “normal” range varies significantly depending on your age and menstrual status.
- Premenopausal Women: The lining fluctuates wildly during the cycle. It can be thin (2-4mm) just after a period and reach 10-16mm before menstruation. So, a 15 mm endometrial thickness in a menstruating woman can be normal if measured just before her period. However, if it is persistently this thick or associated with heavy bleeding, it warrants investigation.
- Postmenopausal Women: The lining should be thin, typically under 4-5mm. A 15 mm endometrial thickness in a postmenopausal woman is considered significantly abnormal and requires a biopsy to rule out pathology.
Uterine Lining Thickness 12mm
Similarly, a uterine lining thickness 12mm is context-dependent.
- During Menstruation: This is thick and may explain heavy clotting.
- Mid-Cycle: This implies the lining is building up.
- Post-Menopause: This is definitely too thick. Any measurement over 4mm or 5mm after menopause typically triggers a diagnostic workup to check for polyps, hyperplasia, or cancer.
Symptoms of Thick Endometrial Lining After Menopause
After menopause, your ovaries stop producing high levels of estrogen, and your periods stop. Consequently, the lining of the uterus should remain thin and inactive.
The primary symptom of a thick lining in this stage is bleeding. Even a single spot of blood after menopause is considered abnormal.
Other subtle signs might include:
- Vaginal discharge (watery or pinkish).
- Pelvic cramping.
- Pain during intercourse.
If you are postmenopausal and the doctor finds a thickened lining (e.g., >5mm), even without bleeding, they may recommend a biopsy to ensure no atypical cells are hiding within the tissue.
Thick Uterine Lining Cause Infertility?
Yes, it can. A healthy endometrium is like a welcoming soil for an embryo. If the lining is too thick (hyperplasia) or contains polyps, the environment becomes hostile.
- Implantation Failure: The embryo struggles to attach to an overgrown or irregular wall.
- Hormonal Chaos: The underlying estrogen dominance preventing ovulation usually accompanies the thick lining, making conception difficult.
- Miscarriage Risk: Even if implantation occurs, the unstable lining may not support the pregnancy, potentially leading to loss.
Treating the underlying hyperplasia and restoring hormonal balance often restores fertility.
How to Reduce Uterine Lining Thickness Naturally
While medical treatment is often necessary, lifestyle changes can support uterine health and help manage estrogen levels.
- Weight Management: Since fat cells produce estrogen, losing excess weight is one of the most effective ways to lower the hormone driving the thickening.
- Dietary Changes: Focus on a low-glycemic, anti-inflammatory diet. Fiber helps the body excrete excess estrogen. Cruciferous vegetables (broccoli, kale) contain compounds that aid estrogen metabolism.
- Exercise: Regular physical activity helps regulate blood sugar and hormones.
- Stress Reduction: Chronic stress impacts cortisol, which in turn affects progesterone production.
Note: Natural remedies are supportive but should not replace professional medical advice, especially if atypical cells are present.
Advanced Non-Surgical Treatment Options: The Interventional Radiology Approach
Traditionally, treatments for severe thickening, fibroids, or adenomyosis involved D&C (scraping the lining) or a Hysterectomy (removing the womb). While effective, these are major surgeries with long recovery times and loss of fertility.
Dr. Samir Abdel Ghaffar offers a revolutionary alternative through Interventional Radiology.
Uterine Artery Embolization (UAE)
For conditions like Adenomyosis and Fibroids that cause the uterine lining to thicken and bleed, UAE is a game-changer.
- How it works: Through a tiny pinhole in the wrist or groin, a catheter is guided to the arteries supplying the uterus. Tiny particles are injected to block the blood flow to the abnormal tissue (fibroids or adenomyosis).
- The Result: The abnormal tissue shrinks, the uterus returns to a more normal size, and the heavy bleeding stops. The healthy uterine tissue remains intact.
- Benefits: No surgery, no general anesthesia, preservation of the uterus, and a very short recovery time.
This approach effectively treats the root causes—like adenomyosis—that lead to the thickened appearance and symptoms, sparing women from the trauma of removing their womb.
Frequently Asked Questions (FAQs)
What happens if the uterus lining is thick?
If left untreated, a thick lining can cause chronic anemia due to heavy blood loss. Long-term, simple hyperplasia can progress to atypical hyperplasia, increasing the risk of cancer.
What does uterine lining thickening feel like?
You don’t “feel” the thickness itself, but you feel the results: heavy, cramping periods, passing large clots, and a sensation of pelvic heaviness or bloating.
When should I worry about endometrium thickness?
You should worry if you have bleeding after menopause, if your periods are consistently heavy (changing protection every hour), or if you are experiencing fertility issues.
Can a thick uterine lining cause weight gain?
The lining itself doesn’t weigh enough to cause noticeable weight gain. However, the hormonal imbalances (like hypothyroidism or PCOS) that cause the thickening often cause weight gain. Also, bloating associated with the menstrual cycle can make you feel heavier.
Is it better to have a thick or thin uterine lining?
Balance is key. Too thin, and you may have fertility issues or low estrogen symptoms. Too thick, and you risk heavy bleeding and cancer. A “normal” thickness appropriate for your cycle phase is best.
What are the red flags for endometriosis?
While different from hyperplasia, endometriosis flags include severe pain that doesn’t respond to painkillers, pain during bowel movements, and pain during sex.
Can thickening of the uterus go away on its own?
If it’s caused by a temporary hormonal blip (like one anovulatory cycle), it might resolve after a period. However, chronic thickening due to PCOS or obesity usually requires intervention to go away.
Can I have a baby with a thick uterus?
If the thickness is due to simple hyperplasia or hormonal imbalance, it can often be treated, restoring fertility. If the “thick uterus” refers to adenomyosis (bulky uterus), pregnancy is harder but still possible, though it may carry higher risks. Treatments like embolization can sometimes help improve the environment for future fertility compared to hysterectomy.
Conclusion: Taking Control of Your Health
A diagnosis of thick lining of uterus symptoms can be unsettling, but it is a manageable condition. Whether it stems from hormonal imbalances, fibroids, or adenomyosis, you have options. You do not always need to rush into major surgery.
Dr. Samir Abdel Ghaffar specializes in accurate diagnosis and minimally invasive treatments using catheterization. By choosing these modern medical insights, you can address the root cause of your heavy periods and pain while preserving your uterus and recovering quickly.
Don’t let heavy bleeding control your life. Seek expert advice today.
You can contact Dr. Samir Abdel Ghaffar through the following:
1. Contact the following numbers in London, UK:
- Clinic number: 00442081442266
- WhatsApp number: 00447377790644
2. Contact the following numbers in Egypt:
- Cairo booking number: 00201000881336
- WhatsApp number: 00201000881336
 العربية
العربية